Are you aware that there exist various methods for testing and monitoring your blood sugar? Glucose levels can be checked using different ways, such as utilizing a blood glucose meter and test strip or opting for a continuous glucose monitor that incorporates a wearable sensor. In recent years, continuous glucose monitoring (CGM) has become a breakthrough technology for people with diabetes. This innovative technology allows people with diabetes to track their blood glucose levels in real-time, providing valuable insights into their overall health and helping to make better treatment decisions. In this article, we will explore “what is continuous glucose monitoring”, delve into its functions, and highlight its importance in helping people with diabetes lead healthier lives.
What is Continuous Glucose Monitoring?
Continuous glucose monitoring (short as CGM) is a wearable device measuring glucose levels in the body on a continuous basis — 24 hours a day. Unlike traditional blood glucose monitoring, which involves periodic finger stick tests, CGM systems provide a more comprehensive and dynamic view of glucose fluctuations throughout the day and night. CGM devices will provide glucose readings at specific intervals, such as every five minutes or so. By constantly monitoring glucose levels, CGM devices offer a wealth of data that can help individuals with diabetes make informed decisions about their diet, medication, and overall diabetes management strategies.
How Does Continuous Glucose Monitoring Work?
Continuous glucose monitoring is a system that provides continuous real-time information about glucose levels in the body. Unlike traditional glucose monitoring methods that provide sporadic snapshots, CGM offers a continuous stream of data, allowing individuals to gain deeper insights into their glucose fluctuations. CGM systems typically consist of three primary components: a tiny glucose sensor, a transmitter, and a receiver or smartphone app.
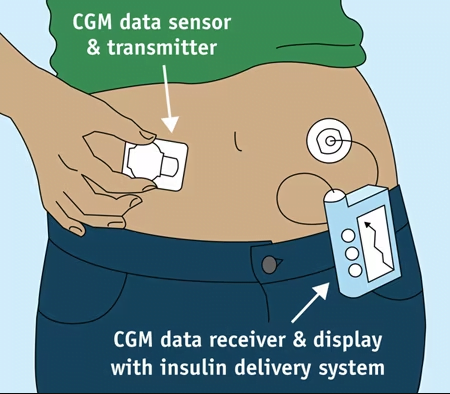
A. Glucose Sensor
At the core of the CGM system lies the glucose sensor. The glucose sensor is a tiny, flexible wire that is inserted beneath the skin, usually in the abdomen. It is designed to measure glucose levels in the interstitial fluid, which surrounds the body’s cells. The sensor uses a tiny electrode to detect the glucose levels in the fluid.
The electrode within the sensor works by employing a process called glucose oxidase, which catalyzes the reaction of glucose with oxygen. This reaction produces a tiny electrical current that the sensor can measure. The magnitude of the current is proportional to the glucose content in the interstitium. By continuously monitoring these electrical signals, the sensor accurately tracks glucose levels throughout the day.
B. Transmitter
The transmitter is a crucial component of the CGM system. It is responsible for collecting the data from the glucose sensor and wirelessly transmitting it to a receiver or a smartphone app. The transmitters are usually connected together with sensors to form a single unit.
Once the glucose sensor measures the glucose levels in the interstitial fluid, it converts the electrical signals into digital data. This data is then wirelessly transmitted by the transmitter using radio frequency or Bluetooth technology. The transmitter sends the glucose readings at regular intervals to the receiver or smartphone app, ensuring that users have access to real-time glucose information.
C. Receiver/Smartphone App
The receiver or smartphone app is the interface between the user and the CGM system. It is the device or application that displays the glucose readings in real time. This provides users with immediate access to their glucose levels. The receiver can be a dedicated device designed explicitly for CGM, while some systems leverage the ubiquity of smartphones and utilize a mobile app as the primary interface.
When the receiver or smartphone app receives the transmitted glucose data, it processes and displays the information in a user-friendly format. Users can customize the display according to their preferences, such as choosing between graphs, charts, or numerical values. Additionally, users can set personalized glucose target ranges within the receiver or app. If glucose levels deviate from these predefined ranges, the system issues alerts, allowing users to take timely action.
Furthermore, the receiver or smartphone app can provide historical data, trends, and patterns based on the collected glucose readings. This feature empowers users to track their glucose fluctuations over time, recognize patterns, and gain valuable insights into their diabetes management.
Who Can Use Continuous Glucose Monitoring?
According to the American Diabetes Association’s abridged 2019 Standards of Medical Care in Diabetes, monitoring blood glucose is key for achieving target blood glucose levels for most people with diabetes. Continuous Glucose Monitoring offers significant benefits to a wide range of individuals with diabetes. While CGM can be beneficial for many, certain groups of people may find it particularly advantageous due to their unique diabetes management needs and challenges. CGM is particularly beneficial for individuals with type 1 diabetes, type 2 diabetes, and gestational diabetes. People who experience frequent hypoglycemia (low blood sugar) or hyperglycemia (high blood sugar), those requiring insulin therapy, or those seeking tighter control over their glucose levels may find CGM highly advantageous. Now let’s explore in more detail who should consider using CGM:
A. Individuals with Type 1 Diabetes
Type 1 diabetes is characterized as an autoimmune condition wherein the immune system of the body targets and eliminates the insulin-producing beta cells situated in the pancreas. People with type 1 diabetes rely on insulin therapy to survive, making precise glucose management crucial. CGM provides real-time data on glucose levels, allowing those with type 1 diabetes to make immediate and informed decisions about insulin dosing, food choices, and physical activity.
B. Individuals with Type 2 Diabetes Requiring Insulin
While people with type 2 diabetes often begin with oral medications or lifestyle interventions, some may eventually require insulin therapy to achieve adequate glucose control. CGM can be immensely beneficial for these individuals, as it helps monitor glucose fluctuations and identify trends that might otherwise go unnoticed. This data empowers patients and healthcare providers to make adjustments to insulin regimens and other treatment strategies for better glycemic outcomes.
C. Pregnant Women with Gestational Diabetes
Gestational diabetes is a temporary form of diabetes that occurs during pregnancy. It can pose risks to both the mother and the baby if not managed effectively. CGM can be a valuable tool for pregnant women with gestational diabetes, enabling them to closely monitor their glucose levels and manage their diet and insulin requirements more efficiently. Tight glucose control during pregnancy can reduce the risk of complications for both the mother and the baby.
D. Individuals with Frequent Hypoglycemia or Hypoglycemia Unawareness
Some people with diabetes experience frequent episodes of hypoglycemia (low blood sugar). CGM systems can provide timely alerts when glucose levels are trending low, helping individuals take preventive action to avoid severe hypoglycemia. Additionally, for those with hypoglycemia unawareness, where they don’t experience typical symptoms of low blood sugar, CGM can serve as a critical safety net.
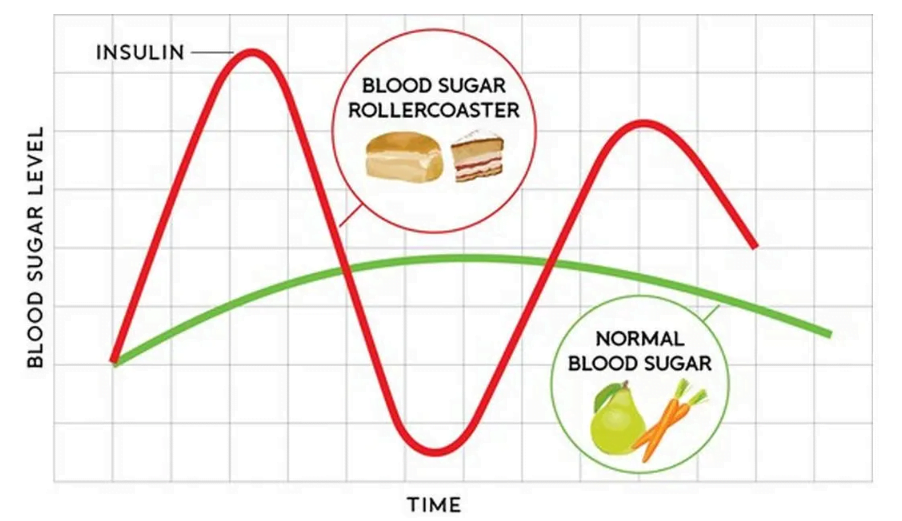
E. Patients Seeking Tighter Glucose Control and Lifestyle Optimization
Individuals aiming for tighter glucose control to prevent diabetes-related complications or to achieve specific health and lifestyle goals can benefit from CGM. CGM enables them to understand how their food choices, exercise, stress, and other factors impact their glucose levels, empowering them to make data-driven decisions for optimal diabetes management.
F. Parents or Caregivers of Children with Diabetes
For parents or caregivers of children with diabetes, CGM provides peace of mind by offering continuous glucose data, even when the child is away. It reduces the need for frequent finger pricks, making diabetes management less intrusive and potentially easing the burden on the child and the caregiver.
What are the benefits of a CGM?
Continuous glucose monitoring offers several advantages over traditional glucose monitoring methods. Here are some key benefits:
A. Real-Time Awareness
CGM provides real-time glucose readings, enabling individuals to promptly respond to fluctuations and make informed decisions about their diabetes management.
B. Trend Analysis
CGM systems generate comprehensive data reports and trends, giving individuals and healthcare professionals valuable insights into glucose patterns over time. This information can help identify potential triggers, adjust medication dosages, and optimize diabetes management strategies.
C. Reduced Hypoglycemia and Hyperglycemia
By providing alerts for high and low glucose levels, CGM systems help individuals avoid severe hypoglycemia or hyperglycemia episodes, promoting better glycemic control and reducing the risk of diabetes-related complications.
D. Improved Quality of Life
CGM technology offers convenience, eliminates the need for frequent finger stick tests, and reduces the guesswork associated with diabetes management. It empowers individuals with diabetes to lead more flexible and active lifestyles.
Continuous Glucose Monitoring has revolutionized diabetes management by providing individuals with real-time insights into their glucose levels, helping them make informed decisions about their treatment and lifestyle choices. With its ability to enhance glucose control, reduce hypoglycemia, and optimize overall diabetes care, CGM technology has paved the way for a brighter future in diabetes management. As technology continues to advance, CGM systems are expected to play an increasingly pivotal role in empowering individuals with diabetes to lead healthier and more fulfilling lives.